Anemia
Highlights
Overview
Anemia is the name applied to many different conditions that are all characterized by an abnormally low number of healthy red blood cells. There are many different causes and types of anemia.
Iron-deficiency anemia, the most common type, is usually treated with dietary changes and iron supplement pills. Other types of anemia, such as those associated with chronic diseases or cancer, may need more aggressive treatment.
Preventing Iron Deficiency in Infants and Toddlers
The American Academy of Pediatrics' updated guidelines for preventing iron deficiency and iron deficiency anemia in infants and young children include:
- Term infants who are healthy and exclusively breastfed should receive an oral iron supplement beginning at 4 months of age. The supplement should be continued until iron-containing solid foods, such as cereals, are introduced. Breast milk itself contains very little iron, but most healthy babies are born with iron stores sufficient for their first 4 months.
- Preterm infants who are breastfed should receive an iron supplement by 1 month of age.
- Formula-fed infants get adequate iron from iron-fortified formula. For all babies, cow’s milk should not be introduced before age 12 months.
- Toddlers ages 1 - 3 years should get their iron from foods, including red meats, iron-rich vegetables, and fruits that are rich in vitamin C. (Vitamin C helps boost iron absorption.)
Introduction
Anemia is an abnormal reduction in red blood cells.
Anemia is not a single disease but a condition, like fever, with many possible causes and many forms. Causes of anemia include nutritional deficiencies, inherited genetic defects, medication-related side effects, and chronic disease. It can also occur because of blood loss from injury or internal bleeding, the destruction of red blood cells, or insufficient red blood cell production. The condition may be temporary or long term, and can manifest in mild or severe forms.
This report focuses on the most common forms of anemia:
- Iron deficiency anemia
- Anemia of chronic disease (ACD)
- Treatment-related anemia (chemotherapy, medication, radiation therapy)
- Megaloblastic anemia (caused by deficiencies in the B vitamins folate, vitamin B12, or both)
Blood
Blood has two major components:
- Plasma is a clear yellow liquid that contains proteins, nutrients, hormones, electrolytes, and other substances. It constitutes about 55% of blood.
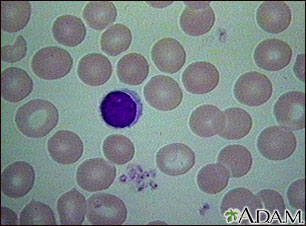
- White and red blood cells and platelets make up the balance of blood. The white cells are the infection fighters for the body. Platelets are necessary for blood clotting. The important factors in anemia, however, are red blood cells.
Red blood cells (RBCs), also known as erythrocytes, carry oxygen throughout the body to nourish tissues and sustain life. Red blood cells are the most abundant cells in our bodies. On average, men have about 5.2 million red blood cells per cubic millimeter of blood, and women have about 4.7 million per cubic millimeter of blood.
Hemoglobin and Iron
Each red blood cell contains 280 million hemoglobin molecules. Hemoglobin is a complex molecule, and it is the most important component of red blood cells. It is composed of protein (globulin) and a molecule (heme), which binds to iron.
In the lungs, the heme component binds to oxygen in exchange for carbon dioxide. The oxygenated red blood cells are then transported to the body's tissues, where the hemoglobin releases the oxygen in exchange for carbon dioxide, and the cycle repeats. The oxygen is used in the mitochondria, the power source within all cells.
Red blood cells typically circulate for about 120 days before they are broken down in the spleen. Most of the iron used in hemoglobin can be recycled from there and reused.
Structure and Shape of Red Blood Cells
Red blood cells -- the erythrocytes -- are extremely small and look something like tiny, flexible discs. This unique shape offers many advantages:
- It provides a large surface area to absorb oxygen and carbon dioxide.
- Its flexibility allows it to squeeze through capillaries, the tiny blood vessels that join the arteries and veins.
Abnormally shaped or sized erythrocytes are typically destroyed and eliminated.
Blood Cell Production (Erythropoiesis)
The actual process of making red blood cells is called erythropoiesis. (In Greek, erythro means "red," and poiesis means "the making of things.") The process of manufacturing, recycling, and regulating the number of red blood cells is complex and involves many parts of the body:
- The body carefully regulates its production of red blood cells so that enough are manufactured to carry oxygen but not so many that the blood becomes thick or sticky (viscous).
- Most of the work of erythropoiesis occurs in the bone marrow. In children younger than 5 years old, the marrow in all the bones of the body is enlisted for producing red blood cells. As a person ages, red blood cells are eventually produced only in the marrow of the spine, ribs, and pelvis.
- If the body needs more oxygen (at high altitudes, for instance), the kidney triggers the release of the hormone erythropoietin (EPO), a hormone that acts in the bone marrow to increase the production of red blood cells.
- The lifespan of a red blood cell is 90 - 120 days. The liver and the spleen remove old red blood cells are removed from the blood by the liver and spleen.
- When old red blood cells are broken down for removal, iron is returned to the bone marrow to make new cells.
Causes
Iron Deficiency Anemia
Iron deficiency anemia occurs when the body lacks mineral iron to produce the hemoglobin it needs to make red blood cells. In general, there are three stages leading from iron deficiency to anemia:
- First, there is an insufficient supply of iron, which causes iron stores in the bone marrow to be depleted. This stage generally has no symptoms.
- Second, iron deficiencies develop and begin to affect hemoglobin production. (Tests will show low hemoglobin and hematocrit levels.)
- Hemoglobin production declines to the point where anemia develops.
Most of the iron used in the body can be recycled from blood and reused. Nevertheless, iron deficiency can occur from a number of conditions.
Inadequate Iron Intake. A healthy diet easily provides enough iron. In general, most people need just 1 mg of extra iron each day. (Menstruating women need 2 mg each day.) This means that lack of iron in the diet is not a common cause of iron deficiency anemia, except in infants. In fact, most American adults may be consuming too much iron in their diet. Iron-poor diets are a cause of anemia only in people with existing risks for iron deficiency. Children who have not yet eaten iron-fortified formulas or iron-enriched cereal may also become anemic.
Blood Loss. Iron deficiencies most commonly occur from internal blood loss due to other conditions that vary in severity. These conditions include:
- Very heavy periods (menorrhagia), the most common causes of anemia in menstruating women
- Peptic ulcers, which may be caused by H. pylori infections, or use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, and naproxen.
- Chronic gastritis, caused by long-term use of NSAIDs, although it is rarely significant enough to cause anemia.
- Duodenal ulcers
- Hemorrhoids, though rare
- Colon polyps
- Colon, stomach, and esophageal cancer
- Bleeding from esophageal varices, often present in alcoholics
Impaired Absorption of Iron. Impaired absorption of iron is caused by:
- Certain intestinal diseases (inflammatory bowel disease, celiac disease)
- Surgical procedures, particularly those involving removal of parts of the stomach and small intestine, can impair the ability of the stomach or intestine to absorb iron. (Such conditions also often impair vitamin B12 absorption.)
- Pica, the craving for non-food substances such as ice, starch, or clay, is a possible cause of iron deficiency in young children. To complicate matters, pica (particularly ice cravings) may also be a symptom, rather than a cause, of anemia.
- Certain intestinal infections, such as hookworm and other parasites.
Genetic Causes. Some people are born with iron deficiency. Certain cases may be due to a mutation of the Nramp2 gene, which regulates a protein responsible for delivering iron to the cells.
Anemia of Chronic Disease (ACD)
Anemia of chronic disease (ACD), also called anemia of chronic inflammation (ACI), is a common condition associated with a wide variety of persistent inflammatory diseases. It can be very severe and require transfusions.
The Inflammatory Process and ACD. In ACD, iron is not efficiently recycled from blood cells, and red blood cells do not survive for as long as normal. In addition, there is impaired response to erythropoietin, the hormone that acts in the bone marrow to increase the production of red blood cells.
Diseases Associated with ACD and Inflammation. The chronic diseases that are associated with this process include:
- Certain cancers. Examples include lymphomas and Hodgkin's disease.
- Autoimmune diseases. Examples include rheumatoid arthritis, systemic lupus erythematosus, inflammatory bowel disease, and polymyalgia rheumatica.
- Long-term infections. Examples include chronic or recurrent urinary tract infections, osteomyelitis, HIV/AIDS, hepatitis C.
- Liver cirrhosis. Cirrhosis can reduce the production of red blood cells. Gastrointestinal bleeding may also contribute to blood loss.
- Heart failure. Many patients with heart failure also have anemia. Anemia is associated with a higher risk of death in patients with heart failure. However, it is unclear whether anemia actually causes or worsens heart failure. Recent research suggests it may actually be a sign (marker) of heart failure. Iron deficiency in heart failure can be due to a number of factors. It may be caused by a lack of nutrients in a person’s diet or by the body’s inability to absorb nutrients from food.
- Chronic kidney disease. The hormone erythropoietin (EPO) is produced in the kidneys and stimulates the bone marrow production of red blood cells. Diseased kidneys do not release sufficient amounts of EPO. Anemia can result and is universal in end-stage renal disease (kidney failure). Chronic kidney disease is a common complication of diabetes.
Not all chronic diseases involve the inflammatory process and anemia. For example, high blood pressure is a chronic disease, but it does not affect red blood cells.
Treatment-Related Anemia
Treatment-related anemia results from the therapies used to treat conditions. For example, anemia is a common side effect of cancer treatments. Chemotherapy and radiation can impair the bone marrow's production of red blood cells and contribute to the extreme fatigue that many patients experience during cancer therapy. Patients with hepatitis C frequently receive combination therapy of ribavirin and interferon; ribavirin can induce anemia. Hepatitis C also affects many patients with HIV or AIDS. In addition to ribavirin, patients with HIV or AIDS can develop anemia as a result of highly active anti-retroviral therapy (HAART) and, in particular, from the drug AZT.
Other medications that increase the risk for anemia are certain antibiotics, some antiseizure medications (phenytoin), immunosuppressive drugs (methotrexate, azathioprine), antiarrhythmic drugs (procainamide, quinidine), and anti-clotting drugs (aspirin, warfarin, clopidogrel, heparin).
Megaloblastic Anemia
Megaloblastic anemia results from deficiencies in the B vitamins folate or vitamin B12 (also called cobalamin). Such deficiencies produce abnormally large (megaloblastic) red blood cells that have a shortened lifespan. Neurologic problems may be associated with vitamin B12 deficiency.
Causes of Vitamin B12 Deficiency. Conditions that cause vitamin B12 deficiencies include:
- Vitamin B12 deficiency from diet is very rare, because the liver stores over a 3-year supply. It usually does not occur even in alcoholism, strict vegetarianism, or in malnourished people with kidney failure or cancer. Since animal products are the chief source, however, true vegan vegetarians may need a supplement, fortified food, or appropriate food selection known to contain adequate amounts of this vitamin
- Pernicious anemia. Pernicious anemia is an autoimmune disease in which antibodies are tricked into attacking stomach cells. This results in impaired production of intrinsic factor (IF), a compound that is critical for absorption of vitamin B12. Pernicious anemia is diagnosed in about 1% of people over age 60, with women having a higher risk than men.
- Complications of gastrointestinal surgery. Surgeries such as stomach bypass or stapling, which remove part or all of the stomach, pose a risk of causing vitamin B12 deficiencies.
- Overgrowth of intestinal bacteria
- Tropical sprue (an acquired malabsorption disease occurring in tropical climates)
Causes of Folate Deficiency. The body stores only about 100 times its daily requirements for folate and can exhaust this supply within about 3 months if the diet is deficient in folate.
- Poor diet coupled with alcoholism is the most common cause of folate deficiency. Alcohol abuse not only contributes to malnutrition but also causes chemical changes that can result in lower folate levels.
- Any condition that disturbs the small intestine and impairs its absorption ability can cause a deficiency. Such disorders include inflammatory bowel disease or celiac sprue (a sensitivity reaction to gluten), as well as gastric bypass weight-loss surgery.
- Parasitic diseases such as giardiasis
- Short bowel syndrome
- Deficiencies can also arise due to high demand for folic acid caused by conditions such as cancer, pregnancy, severe psoriasis, severe hyperthyroidism, and hemolytic anemia.
- Some drugs, including phenytoin, methotrexate, trimethoprim, and triamterene, may also hinder folate absorption.
Risk Factors
Among Americans with iron deficiency anemia, young children have the highest risk followed by premenopausal women. Adolescent and adult men and postmenopausal women have the lowest risk. Men, in fact, are at risk for iron overload, probably because of their high meat intake and minimal iron loss.
Infants and Children
Up to 20% of American children and 80% of children in developing countries become anemic at some point during their childhood and adolescence. Iron deficiency is the most common cause in children, but other forms of anemia, including hereditary blood disorders, can also cause anemia in this population.
Hispanic American children have double the rates of iron deficiency as African-American and Caucasian children. Children in lower-income homes are at higher risk than those in higher income homes. However, children in any income group can develop iron deficiency.
Children need to absorb an average of 1 mg per day of iron to keep up with the needs of their growing bodies. Since children only absorb about 10% of the iron they eat, most children need to receive 8 - 10 mg of iron per day. However, breast milk contains very little iron. Babies who are exclusively breastfed should get a daily oral iron supplement starting at age 4 months and continued until iron-rich solid foods are introduced.
An iron-poor diet is a common cause of iron deficiency. Drinking too much cow's milk (usually more than 2 cups per day) is a common cause of iron deficiency in young children because cow’s milk contains little iron and can get in the way of iron absorption. Cow's milk also can cause problems in the intestine that lead to blood loss and increased risk of anemia. Babies should not get cow’s milk before they are 12 months old.
Iron deficiency most commonly affects babies 9 - 24 months old. All babies should have a screening test for iron deficiency at around age 12 months. Babies born prematurely may need to be tested earlier. Other factors associated with iron-deficiency anemia in infants and small children include:
- Stopping breastfeeding too early or using formula that isn't iron-fortified.
- Bottle-feeding too long. Bottle-fed babies who are 7 - 9 months old should be weaned from bottles and given sippy cups. By the age of 12 months, all children should be using a cup instead of a bottle.
- Toddlers’ preferences for iron-poor food. Parents should make sure that their children eat iron-rich foods such as beans, meat, fortified cereals, eggs, and green leafy vegetables
Premenopausal Women
Up to 10% or more of adolescent and adult women under age 49 years are iron deficient. Anemia among premenopausal women typically occurs from:
- Heavy menstruation for longer than 5 days
- Abnormal uterine bleeding, such as from fibroids
- Pregnancy (see below)
Older Adults
Causes of anemia in adults age 65 years and older include nutritional deficiencies, chronic inflammatory disease, and chronic renal disease.
Alcoholism
People with alcoholism are at risk for anemia both from internal bleeding as well as folate- and vitamin B deficiency-related anemias.
Iron-Poor Diets
Although most Americans probably consume too much iron in their diets, some people may be at risk for diet-related iron deficiencies, including:
- People whose diets are high in processed foods and lack any meat.
- Strict vegetarians. Vegetarians who avoid all animal products may have a slightly higher risk for deficiencies in iron and some B vitamins. Although dried beans and green vegetables often contain iron, it is less easily absorbed from plants than from meat. Fortunately, most commercial cereals and grain products are fortified with an easily absorbed form of vitamin B12 and with folic acid (the synthetic form of folate).
Although nutritional iron-deficiency anemia has declined in industrialized nations, it still affects about 2 billion people worldwide. Even in the U.S., iron deficiency is the most prevalent nutritional deficiency. It is highly associated with poverty. People in lower socioeconomic groups have double the risk of those who are middle or upper class.
Chronic or Critical Illnesses
Anyone with a chronic disease that causes inflammation or bleeding is at risk for anemia. Critical illness in the intensive care unit is also highly associated with anemia.
Pregnancy
Pregnancy is associated with fluid retention, which in turn may produce high volumes of plasma (the fluid component of blood). This process can dilute red blood cells, which may lead to lower hemoglobin and hematocrit levels. These changes by themselves can be considered a normal alteration of pregnancy. However, other factors increase the risk for anemia during pregnancy:
- Pregnancy increases the body's demand for folic acid, which poses a risk for folate deficiency and, therefore, megaloblastic anemia.
- Pregnancy increases the body's demand for iron, thus posing a risk for iron deficiency anemia. Pregnant women need 27 mg of iron per day.
- During delivery, heavy bleeding or multiple births can cause postpartum anemia. Postpartum anemia can last 6 - 12 months after giving birth.
Complications
Most cases of anemia are mild, including those that occur as a result of chronic disease. Nevertheless, even mild anemia can reduce oxygen transport in the blood, causing fatigue and a diminished physical capacity. Moderate-to-severe iron-deficiency anemia is known to reduce endurance. Some studies indicate that even iron deficiency without anemia can produce a subtle but still lower capacity for exercise.
Because a reduction in red blood cells decreases the ability to absorb oxygen from the lungs, serious problems can occur in prolonged and severe anemia that is not treated. Anemia can lead to secondary organ dysfunction or damage, including heart arrhythmias and heart failure.
Effects of Anemia in Pregnant Women
Pregnant women with significant anemia may have an increased risk for poor pregnancy outcomes, particularly if they are anemic in the first trimester. Mild-to-moderate anemia does not pose any increased risk.
Complications from Anemia in Children and Adolescents
In children, severe anemia can impair growth and motor and mental development. Children may exhibit a shortened attention span and decreased alertness. Children with severe iron-deficiency anemia may also have an increased risk for stroke.
Effects of Anemia in the Elderly
Anemia is common in older people and can have significantly more severe complications than anemia in younger adults. Effects of anemia in the elderly include decreased strength and increased risk for falls. Anemia may have adverse effects on the heart and increase the severity of cardiac conditions, including reducing survival rates from heart failure and heart attacks. Even mild anemia may possibly lead to cognitive impairment or worsen existing dementia.
Effects of Vitamin B12 Deficiencies and Pernicious Anemia
In addition to anemia, vitamin B12 deficiency can cause neurologic damage, which can be irreversible if it continues for long periods without treatment.
Anemia in Patients with Cancer
Anemia is particularly serious in cancer patients. In people with many common cancers, the presence of anemia is associated with a shorter survival time.
Anemia in Patients with Kidney Disease
Anemia is associated with higher mortality rates and possibly heart disease in patients with kidney disease.
Anemia in Patients with Heart Failure
The combination of anemia and heart failure can increase the risk of hospitalization or death. Patients with heart failure whose hemoglobin levels decline do worse than patients with stable levels.
Effects of Excess Iron
Patients with certain types of anemia need frequent blood transfusions. These transfusions can cause iron overload. [For more information, see "Transfusions" in Treatment section of this report.]
Symptoms
Symptoms of anemia vary depending on the severity of the condition. Anemia may occur without symptoms and be detected only during a medical examination that includes a blood test. When they occur, symptoms may include:
- Weakness and fatigue are the most common symptoms of anemia. Even iron deficiency without anemia can reduce working capacity in some people.
- Shortness of breath on exertion
- Rapid heartbeat
- Lightheadedness or dizziness
- Headache
- Ringing in the ears (tinnitus)
- Irritability and other mood disturbances
- Pale skin (however, healthy-looking skin color does not rule out anemia if a patient has risk factors and other symptoms of anemia)
- Mental confusion
- Loss of sexual drive
- Restless legs syndrome may be a symptom of iron deficiency
Unusual Symptoms
Pica. One odd symptom, which in some cases is also a cause of iron deficiency, is pica. This is the habit of eating unusual substances, such as ice (called pagophagia), clay, cardboard, foods that crunch (such as raw potatoes, carrots, or celery), or raw starch. The pica often stops, particularly in children, when iron supplements are given.
The finding of pica in adults, most often ice chips or cornstarch, is known to be associated with iron deficiency anemia. However, pica can be difficult to detect because patients are often ashamed to admit to such cravings.
Symptoms of Megaloblastic Anemia and its Causes
Symptoms of Megaloblastic Anemia. The symptoms of megaloblastic anemia from vitamin B12 or folic acid deficiencies include not only standard anemic symptoms but also:
- Inflammation of the mouth (stomatitis)
- Inflammation of the tongue (glossitis), which involves shrinkage at the surface and edges of the tongue
Over time, psychiatric and neurologic problems develop. Vitamin B12 deficiencies can cause neurologic symptoms (numbness and tingling, depression, memory loss, and irritability).
Symptoms of Pernicious Anemia. Early neurologic symptoms of pernicious anemia, which is a form of megaloblastic anemia, are due to B12 deficiency. They include numbness and tingling, depression, memory loss, and irritability. Advanced nerve damage can cause loss of balance and staggering, confusion, dementia, spasticity, loss of bladder control, and erectile dysfunction. Folic acid deficiency does not cause neurologic damage, although people with this deficiency can be irritable, forgetful, and experience personality changes.
Diagnosis
Because anemia may be the first symptom of a serious illness, it is very important to determine its cause. This may be difficult, particularly in the elderly, malnourished, or people with chronic diseases, whose anemia may be caused by one or more factors. A detailed medical, personal, and dietary history should report:
- Any family or personal history of anemia
- A history of gallbladder disease, jaundice, or enlarged spleen
- Heavy menstrual bleeding in women
- Any occurrence of blood in the stool or other signs of internal bleeding
- Dietary history, particularly in people who are elderly, poor, or both
The doctor should examine the patient carefully, especially checking for swollen lymph nodes, an enlarged spleen, and pale skin and nail color.
A complete blood count (CBC) blood test is performed to determine the presence of anemia. Other iron status blood tests are also used.
Complete Blood Count (CBC)
A complete blood count (CBC) is a panel of tests that measures red blood cells, white blood cells, and platelets. For diagnosis of anemia, the CBC provides critical information on the size, volume, and shape of red blood cells (erythrocytes). CBC results include measurements of hemoglobin, hematocrit, and mean corpuscular volume.
Hemoglobin. Hemoglobin is the iron-bearing and oxygen-carrying component of red blood cells. The normal value for hemoglobin varies by age and gender. Anemia is generally considered when hemoglobin concentrations fall below 11 g/dL for pregnant women, 12 g/dL for non-pregnant women, and 13 g/dL for men.
The severity of anemia is categorized by the following hemoglobin concentration ranges:
- Mild anemia is considered when hemoglobin is between 9.5 - 13.0 g/dL
- Moderate anemia is considered when hemoglobin is between 8.0 - 9.5 g/dL
- Severe anemia is considered for hemoglobin concentrations below 8.0 g/dL
Hematocrit. Hematocrit is the percentage of blood composed of red blood cells. People with a high volume of plasma (the liquid portion of blood) may be anemic even if their blood count is normal because the blood cells have become diluted. Like hemoglobin, a normal hematocrit percentage depends on age and gender. In general, doctors diagnose anemia when hematocrit falls below:
- 33% for children 6 months - 5 years
- 35% for children 5 - 12 years
- 36% for children 12 - 15 years
- 39% for adult men
- 36% for adult non-pregnant women
- 33% for adult pregnant women
Other hemoglobin measurements, such as mean corpuscular hemoglobin (MCH) and mean corpuscular hemoglobin concentration (MCHC) may also be calculated.
Mean Corpuscular Volume. Mean corpuscular volume (MCV) is a measurement of the average size of red blood cells. The MCV increases when red blood cells are larger than normal (macrocytic) and decreases when red blood cells are smaller than normal (microcytic). Macrocytic cells can be a sign of anemia caused by vitamin B12 deficiency, while microcytic cells are a sign of iron-deficiency anemia or thalassemias.
Other Iron Status Blood Tests
Serum Ferritin. Ferritin is a protein that binds to iron and helps to store iron in the body. Low levels typically mean reduced iron stores. Normal values are generally 12 - 300 ng/mL for men and 12 - 150 ng/mL for women. Lower than normal levels of ferritin are a sign of iron-deficiency anemia, while higher than normal levels may indicate hemolytic anemia or megaloblastic anemia.
Serum Iron. Serum iron measures the amount of iron in the blood. A normal serum iron is 60 - 170 mcg/dL. Lower levels may indicate iron-deficiency anemia or anemia of chronic disease, while higher levels may indicate hemolytic anemia or vitamin B12 deficiency.
Total Iron Binding Capacity. Total iron binding capacity (TIBC) measures the level of transferrin in the blood. Transferrin is a protein that carries iron in the blood. TIBC calculates how much or how little the transferrin in the body is carrying iron. A higher than normal TIBC is a sign of iron-deficiency anemia. A lower than normal level may indicate anemia of chronic disease, sickle cell, pernicious anemia, or hemolytic anemia.
Reticulocyte Count. Reticulocytes are young red blood cells, and their count reflects the rate of red blood cell production. The upper normal limit is about 100,000/mL. A low count, when bleeding isn't the cause, suggests production problems in the bone marrow. An abnormally high count indicates that red blood cells are being destroyed in high numbers and indicates hemolytic anemia. Recent research suggests that the reticulocyte hemoglobin content (CHr) test may be more accurate than a standard hemoglobin test for detecting iron deficiency in infants.
Vitamin Deficiencies. The doctor may order tests for vitamin B12 and folate levels. The Schilling test is used to determine whether the body absorbs vitamin B12 normally.
Other Diagnostic Tests
If internal bleeding is suspected as the cause of anemia, the gastrointestinal tract is usually the first possible source. A diagnosis in these cases can often be made if the patient has noticed blood in the stools, which can be black and tarry or red-streaked. Often, however, bleeding may be present but not visible. If so, the patient needs stool tests for this hidden (occult) blood. The patient may need additional tests to diagnose the precipitating condition. Endoscopy, in which a fiber optic tube is used to view into the gastrointestinal tract, is helpful in many patients, particularly when the source of bleeding is unclear. A colonoscopy may also be recommended to rule out colorectal cancer.
If the patient's diet suggests low iron intake and other causes cannot be established using inexpensive or noninvasive techniques, the patient may simply be given a monthly trial of iron supplements. If the patient fails to respond, further evaluation is needed.
Dietary Factors
Iron found in foods is either in the form of heme iron (attached to hemoglobin molecule) or non-heme iron:
- Heme Iron. Foods containing heme iron are the best sources for increasing or maintaining healthy iron levels. Such foods include (in decreasing order of iron-richness) clams, oysters, organ meats, beef, pork, poultry, and fish.
- Non-Heme Iron. Non-heme iron is less well-absorbed. About 60% of the iron in meat is non-heme (although meat itself helps absorb non-heme iron). Eggs, dairy products, and iron-containing vegetables have only the non-heme form. Such vegetable products include dried beans and peas, iron-fortified cereals, bread, and pasta products, dark green leafy vegetables (such as chard, spinach, mustard greens, and kale), dried fruits, nuts, and seeds.
The absorption of non-heme iron often depends on the food balances in meals. The following foods and cooking methods can enhance absorption of iron:
- Meat and fish not only contain heme iron -- the best form for maintaining stores -- but they also help absorb non-heme iron.
- Increasing intake of vitamin-C rich foods, such as orange juice, may enhance absorption of non-heme iron, although it is not clear if it improves iron stores in iron-deficient people. In any case, vitamin-C rich foods are healthy and include broccoli, cabbage, citrus fruits, melon, tomatoes, and strawberries.
- Riboflavin (vitamin B2) may help enhance the response of hemoglobin to iron. Food sources include dairy products, liver, and dried fortified cereals.
- Cooking methods can enhance iron stores. Cooking in cast iron pans and skillets can help increase the iron content of food.
- Vitamins B12 and folate are important for prevention of megaloblastic anemia and for good health in general. The only natural dietary sources of B12 are animal products, such as meats, dairy products, eggs, and fish (clams and oily fish are very high in B12). As is the case with other B vitamins, however, B12 is added to commercial dried cereals. The recommended daily allowance (RDA) for adults is 2.4 mcg a day. Deficiencies are rare in young people, although the elderly may have trouble absorbing natural vitamin B12 and require the more easily absorbed synthetic form of B12 from fortified foods or supplements.
- Folate is found in avocado, bananas, orange juice, cold cereal, asparagus, fruits, green, leafy vegetables, dried beans and peas, and yeast. The synthetic form, folic acid, is now added to commercial grain products. Vitamins are usually made from folic acid, which is about twice as potent as folate. The recommended daily amount of folic acid or folate for teenagers and adults is 400 mcg. Women who are pregnant need 600 mcg per day and women who are breastfeeding need 500 mcg daily.
Recommended Daily Allowance for Iron
The Recommended Daily Allowance (RDA) of iron for people who are not iron deficient varies by age group and other risk factors. (Iron supplements are rarely recommended in people without evidence of iron deficiency or anemia.) The RDA for iron intake is:
- Infants 0 - 6 months: 0.27 mg
- Infants 7 - 12 months: 11 mg
- Children 1 - 3 years old: 7 mg
- Children 4 - 8 years old: 10 mg
- Children 9 -13 years old: 8 mg
- Teenage boys (14 - 18 years): 11 mg
- Teenage girls (14 - 18 years): 15 mg
- Men 19 - 50 years old: 8 mg
- Women 19 - 50 years old: 18 mg
- Pregnant women: 27 mg
- Older men and women (over age 50): 8 mg
Preventing Anemia in Infants and Small Children
The main source of iron for an infant from birth to 1 year of age is from breast milk, iron-fortified infant formula, or cereal.
Breastfeeding and Iron-Supplemented Formulas. Mothers should be encouraged to breastfeed their babies for their first year. The American Academy of Pediatrics (AAP) recommends exclusively breastfeeding for a minimum of 4 months, but preferably 6 months, then gradually adding solid foods while continuing to breastfeed until at least the baby’s first birthday. Because human breast milk contains very little iron, the AAP recommends that full-term healthy infants receive a daily oral iron supplement of 1 mg/kg beginning at age 4 months and continuing until iron-rich complementary foods, such as iron-fortified cereals, are introduced. Preterm infants who are breastfed should receive an iron supplement of 2 mg/kg by the time they are 1 month old.
Infants who are not breastfed should receive iron-fortified formulas (4 - 12 mg/L for their first year of life). Parents should discuss the best formula with their doctor. The AAP does not recommend cow’s milk for children under 1 year old. The baby will begin drinking less formula or breast milk once solid foods become a source of nutrition. At 8 - 12 months of age, a baby will be ready to try strained or finely chopped meats. When cereals are begun, they should be iron fortified.
Recommendations for Toddlers. Toddlers who did not have iron supplements during infancy should be checked for iron deficiency. After the first year, children should be given a varied diet that is rich in sources of iron, B vitamins, and vitamin C. Good sources of iron include iron-fortified grains and cereals, egg yolks, red meat, potatoes (cooked with skin on), tomatoes, molasses, and raisins. Milk does not contain enough iron and can decrease children's appetite for iron-rich foods. Toddlers older than 1 year should not drink more than 2 cups of milk a day. Fruits that are rich in vitamin C can help boost iron absorption. Most children will receive adequate iron from a well-balanced diet, but some toddlers may benefit from liquid supplements or chewable multivitamins.
Treatment
Oral iron supplements are the best way to restore iron levels for people who are iron deficient, but they should be used only when dietary measures have failed. However, iron supplements cannot correct anemias that are not due to iron deficiency.
Iron replacement therapy can cause gastrointestinal problems, sometimes severe ones. Excess iron may also contribute to heart disease, diabetes, and certain cancers. Doctors generally advise against iron supplements in anyone with a healthy diet and no indications of iron deficiency anemia.
Treatment of Anemia of Chronic Disease. In general, the best treatment for anemia of chronic diseases is treating the disease itself. In some cases, iron deficiency accompanies the condition and requires iron replacement. Erythropoietin, most often administered with intravenous iron, is used for some patients.
Oral Iron Supplements
Supplement Forms. There are two forms of supplemental iron: ferrous and ferric. Ferrous iron is better absorbed and is the preferred form of iron tablets. Ferrous iron is available in three forms: ferrous fumarate, ferrous sulfate, and ferrous gluconate.
The label of an iron supplement contains information both on the tablet size (which is typically 325 mg) and the amount of elemental iron contained in the tablet (the amount of iron that is available for absorption by the body.) When selecting an iron supplement, it is important to look at the amount of elemental iron.
A 325 mg iron supplement contains the following amounts of elemental iron depending on the type of iron:
- Ferrous fumarate. 108 mg of elemental iron
- Ferrous sulfate. 65 mg of elemental iron
- Ferrous gluconate. 35 mg of elemental iron
Dosage. Depending on the severity of your anemia, as well as your age and weight, your doctor will recommend a dosage of 60 - 200 mg of elemental iron per day. This means taking one iron pill 2 - 3 time during the day. Make sure your doctor explains to you how many pills you should take in a day and when you should take them. Never take a double dose of iron.
Side Effects and Safety. Common side effects of iron supplements include:
- Constipation and diarrhea are very common. They are rarely severe, although iron tablets can aggravate existing gastrointestinal problems such as ulcers and ulcerative colitis.
- Nausea and vomiting may occur with high doses, but taking smaller amounts of medicine can control the problem. Switching to ferrous gluconate may help some people with severe gastrointestinal problems.
- Black stools are normal when taking iron tablets. In fact, if they do not turn black, the tablets may not be working effectively. This problem tends to be more common with coated or long-acting iron tablets.
- If the stools are tarry looking as well as black, if they have red streaks, or if cramps, sharp pains, or soreness in the stomach occur, gastrointestinal bleeding may be causing the iron deficiency. The patient should call the doctor promptly.
- Acute iron poisoning is rare in adults but can be fatal in children who take adult-strength tablets. Keep iron supplements out of the reach of children. If your child swallows an iron pill, immediately contact a poison control center.
Other Tips for Safety and Effectiveness. Other tips for taking iron are as follows:
- For best absorption, iron should be taken between meals. Iron may cause stomach and intestinal disturbances, however. Low doses of ferrous sulfate can be taken with food and are still absorbed but with fewer side effects.)
- Drink a full 8 ounces of fluid with an iron pill. Taking orange juice with an iron pill can help increase iron absorption. (Some doctors also recommend taking a vitamin C supplement with the iron pill.)
- If constipation becomes a problem, take a stool softener such as docusate sodium (Colace).
- Certain medications, including antacids, can reduce iron absorption. Iron tablets may also reduce the effectiveness of other drugs, including the antibiotics tetracycline, penicillin, and ciprofloxacin and the Parkinson's disease drugs methyldopa, levodopa, and carbidopa. At least 2 hours should elapse between doses of these drugs and iron supplements.
- Avoid taking milk, caffeine, antacids, or calcium supplements at the same time as an iron pill as they can interfere with iron absorption.
- Tablets should be kept in a cool place. (Bathroom medicine cabinets may be too warm and humid, which may cause the pills to disintegrate.)
The hematocrit should return to normal after 2 months of iron therapy. However, iron supplementation should be continued for another 6 - 12 months to replenish the body's iron stores in the bone marrow.
Intravenous or Injected Iron
In some cases, iron is administered through muscular injections or intravenously. Intravenous iron has the advantage of causing less gastrointestinal discomfort and inconvenience. It may be in the form of iron dextran (Dexferrum, InFed), sodium ferric gluconate complex in sucrose (Ferrlecit), or iron sucrose (Venofer). Ferrlecit or Venofer are equally effective and generally safer than iron dextran.
Candidates. The injected or intravenous forms should be limited to the following patients with iron deficiency:
- People with iron deficiency anemia in whom oral therapy has clearly failed.
- Patients with bleeding disorders in which blood loss continues to exceed the rate at which oral iron is absorbed.
- In emergencies, when people need red blood cells but transfusion is not appropriate or available.
- In people with serious gastrointestinal disorders, such as inflammatory bowel disease, who cannot take iron therapy by mouth.
- People undergoing hemodialysis who receive supplemental erythropoietin therapy. Sodium ferric gluconate complex in sucrose (Ferrlecit) or iron sucrose (Venofer) is specifically approved as first-line therapy for these patients.
Certain patients, even if they meet these qualifications, may not be appropriate candidates or should be monitored closely for complications. They include:
- Patients with any underlying autoimmune disease.
- Malnourished patients who also have an underlying infection.
- Patients who are at risk for iron overload.
Side Effects. Some side effects differ depending on how the iron is administered and include the following:
- Muscular injections include pain at the site.
- Intravenous administration can cause pain in the vein, flushing, and metallic taste, all of which are brief.
For both methods, side effects and serious complications can include:
- Blood clots
- Fever
- Joint aches
- Headache
- Rashes
- A delayed reaction of joint and muscle aches, headache, and malaise occurs 1 - 2 days after the infusion (most commonly with iron dextran) in about 10% of patients. These symptoms respond quickly to NSAIDs, such as ibuprofen or naproxen, in most people.
- Iron toxicity. Symptoms include nausea, dizziness, and a sudden drop in blood pressure. Sodium ferric gluconate in sucrose (Ferrlecit) or iron sucrose (Venofer) may pose a lower risk for toxicity than iron dextran.
- Allergic reactions. Allergic reactions that occur with intravenous iron can be very serious and, in rare cases, even fatal. Iron dextran appears to pose a much higher risk than sodium ferric gluconate complex in sucrose or iron sucrose, although allergic reactions can also occur with the latter forms.
Oral and injected iron should never be given at the same time. Intravenous iron therapy may be appropriate for some pregnant women who meet these requirements, depending on the pregnancy term and other factors.
Blood Transfusions
Transfusions are used to replace blood loss due to injuries and during certain surgeries. They are also commonly used to treat severely anemic patients who have thalassemia, sickle cell disease, myelodysplastic syndromes, or other types of anemia. Some patients require frequent blood transfusions. Iron overload can be a side effect of these frequent blood transfusions. If left untreated, iron overload can lead to liver and heart damage.
Iron chelation therapy is used to remove the excess iron caused by blood transfusions. Patients take a drug that binds to the iron in the blood. The excess iron is then removed from the body by the kidneys.
Deferasirox (Exjade) is a drug that is given as a once-daily treatment for iron overload due to blood transfusions. It does not require injections. Patients mix the deferasirox tablets in liquid and drink the medicine.
Erythropoiesis-Stimulating Drugs
Erythropoietin is the hormone that acts in the bone marrow to increase the production of red blood cells. It has been genetically engineered as recombinant human erythropoietin (rHuEPO) and is available as epoetin alfa (Epogen, Procrit, and Eprex). Novel erythropoiesis stimulating protein (NESP), also called darbepoetin alfa (Aranesp), lasts longer in the blood than epoetin alfa and requires fewer injections. These medications are also called “erythropoiesis-stimulating drugs.”
Levels of erythropoietin are reduced in anemia of chronic disease. Injections of synthetic erythropoietin can help increase the number of red blood cells in order to avoid receiving blood transfusions. Synthetic erythropoietin can cause serious side effects, including blood clots, and is approved only for treating patients with anemia related to the following conditions:
- Cancer. For select patients, erythropoietin is used to treat the anemia associated with chemotherapy.
- Chronic kidney disease. Erythropoietin is an important anemia treatment for patients with chronic kidney disease, including those with end-stage renal disease who are on dialysis.
- HIV/AIDS. Erythropoietin helps treat the anemia caused by zidovudine (AZT) therapy.
Erythropoiesis-Stimulating Drugs and Cancer. Erythropoietin may be used to treat anemia caused by chemotherapy. Erythropoietin treatment does not help prolong survival, but can improve quality of life during cancer treatment by improving anemia.
However, these drugs can shorten lifespan and cause some tumors to grow faster. In general, the lowest effective dose should be used. The risks of early death and increased tumor growth are greatest when these drugs are used to boost the hemoglobin level to 10 - 12 g/dL or higher. The American Society of Clinical Oncology and the American Society of Hematology recommend starting erythropoietin only if a patient’s hemoglobin level is less than 10 g/dL.)
Discuss with your doctor whether an erythropoiesis-stimulating drug is appropriate for you.
Erythropoiesis-Stimulating Drugs and Chronic Kidney Disease. For patients with chronic kidney disease or kidney failure, the FDA currently recommends that erythropoiesis-stimulating drugs be used to maintain hemoglobin levels between 10 - 12 g/dL. (The exact level within this range varies by individual.) There is a greater risk of death and serious cardiovascular events, such as heart attack, stroke, and heart failure when these drugs are used to achieve higher hemoglobin levels (13.5 - 14g/dL) compared to lower hemoglobin levels (10 - 11.3 g/dL).
Warning Symptoms. Contact your doctor if you have any of the following symptoms while being treated with an erythropoiesis-stimulating drug:
- Pain or swelling in the legs
- Worsening in shortness of breath
- Increases in blood pressure (be sure to regularly monitor your blood pressure)
- Dizziness or loss of consciousness
- Extreme fatigue
- Blood clots in hemodialysis vascular access ports
Vitamin Replacement for Megaloblastic Anemia
Megalobastic anemia is marked by abnormally large red blood cells. (Pernicious anemia is a type of megaloblastic anemia). It is caused by impaired absorption or insufficient intake of vitamin B12 or folate. If folate deficiency is responsible, treatment usually involves taking a daily oral folic acid supplement for at least several months as well as increasing intake of foods rich in folate. When vitamin B12 deficiency is responsible, vitamin B12 may be administered in tablets, injections of cyanocobalamin or hydroxocobalamin, or as a nasal spray.
Resources
- www.anemia.org -- National Anemia Action Council
- www.nhlbi.nih.gov -- National Heart, Lung and Blood Institute
- www.irondisorders.org -- Iron Disorders Institute
- www.healthychildren.org -- Healthy Children (American Academy of Pediatrics)
References
Alleyne M, Horne MK, Miller JL. Individualized treatment for iron-deficiency anemia in adults. Am J Med. 2008 Nov;121(11):943-8.
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 95: anemia in pregnancy. Obstet Gynecol. 2008 Jul;112(1):201-7.
Baker RD, Greer FR; Committee on Nutrition American Academy of Pediatrics. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0-3 years of age). Pediatrics. 2010 Nov;126(5):1040-50. Epub 2010 Oct 5.
Bennett CL, Silver SM, Djulbegovic B, Samaras AT, Blau CA, Gleason KJ, et al. Venous thromboembolism and mortality associated with recombinant erythropoietin and darbepoetin administration for the treatment of cancer-associated anemia. JAMA. 2008 Feb 27;299(8):914-24.
Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Recombinant human erythropoiesis-stimulating agents and mortality in patients with cancer: a meta-analysis of randomised trials. Lancet. 2009 May 2;373(9674):1532-42.
Brotanek JM, Gosz J, Weitzman M, Flores G. Iron deficiency in early childhood in the United States: risk factors and racial/ethnic disparities. Pediatrics. 2007 Sep;120(3):568-75.
Bunn H. Approach to the anemias. In: Goldman L, Schafer AI, eds. Cecil Medicine. 24th ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 161.
Clement FM, Klarenbach S, Tonelli M, Johnson JA, Manns BJ. The impact of selecting a high hemoglobin target level on health-related quality of life for patients with chronic kidney disease: a systematic review and meta-analysis. Arch Intern Med. 2009 Jun 22;169(12):1104-12.
Goddard AF, James MW, McIntyre AS, Scott BB; British Society of Gastroenterology. Guidelines for the management of iron deficiency anaemia. Gut. 2011 Oct;60(10):1309-16. Epub 2011 May 11..
Groenveld HF, Januzzi JL, Damman K, van Wijngaarden J, Hillege HL, van Veldhuisen DJ, et al. Anemia and mortality in heart failure patients a systematic review and meta-analysis. J Am Coll Cardiol. 2008 Sep 2;52(10):818-27.
Heird WC. The feeding of infants and children. In: Kliegman RM, Behrman RE, Jenson HB, Stanton BF, eds. Nelson Textbook of Pediatrics. 18th ed. Philadelphia, Pa: Saunders Elsevier; 2007:chap 42.
Janus J, Moerschel SK. Evaluation of anemia in children. Am Fam Physician. 2010 Jun 15;81(12):1462-71.
Killip S, Bennett JM, Chambers MD. Iron deficiency anemia. Am Fam Physician. 2007 Mar 1;75(5):671-8.
KDOQI. KDOQI Clinical Practice Guideline and Clinical Practice Recommendations for anemia in chronic kidney disease: 2007 update of hemoglobin target. Am J Kidney Dis. 2007 Sep;50(3):471-530.
Ludwig H, Crawford J, Osterborg A, Vansteenkiste J, Henry DH, Fleishman A, et al. Pooled analysis of individual patient-level data from all randomized, double-blind, placebo-controlled trials of darbepoetin alfa in the treatment of patients with chemotherapy-induced anemia. J Clin Oncol. 2009 Jun 10;27(17):2838-47. Epub 2009 Apr 20.
Mabry-Hernandez IR. Screening for iron deficiency anemia -- including iron supplementation for children and pregnant women. Am Fam Physician. 2009 May 15;79(10):897-8.
Pfeffer MA, Burdmann EA, Chen CY, Cooper ME, de Zeeuw D, Eckardt KU, et al. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med. 2009 Nov 19;361(21):2019-32. Epub 2009 Oct 30.
Rizzo JD, Brouwers M, Hurley P, Seidenfeld J, Arcasoy MO, Spivak JL, et al. American Society of Hematology/American Society of Clinical Oncology clinical practice guideline update on the use of epoetin and darbepoetin in adult patients with cancer. Blood. 2010 Nov 18;116(20):4045-59. Epub 2010 Oct 25
Rodgers GM 3rd, Becker PS, Bennett CL, Cella D, Chanan-Khan A, Chesney C, et al. Cancer- and chemotherapy-induced anemia. National Comprehensive Cancer Network. 2010.v.2.
Unger EF, Thompson AM, Blank MJ, Temple R. Erythropoiesis-stimulating agents - time for a reevaluation. N Engl J Med. 2010 Jan 6: 10.1056/nejmp0912328
|
Review Date:
2/7/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |








